Why in the News?
- With antimicrobial resistance on the rise, the Union Health Ministry has urged doctors to write down the exact reason when prescribing antibiotics.
What’s in Today’s Article?
- About AMR (Meaning, Causes, Intervention Strategies, Steps Taken by Govt.)
- News Summary
About Antimicrobial Resistance (AMR):
- Antimicrobials – including antibiotics, antivirals, antifungals and antiparasitic – are medicines used to prevent and treat infections in humans, animals and plants.
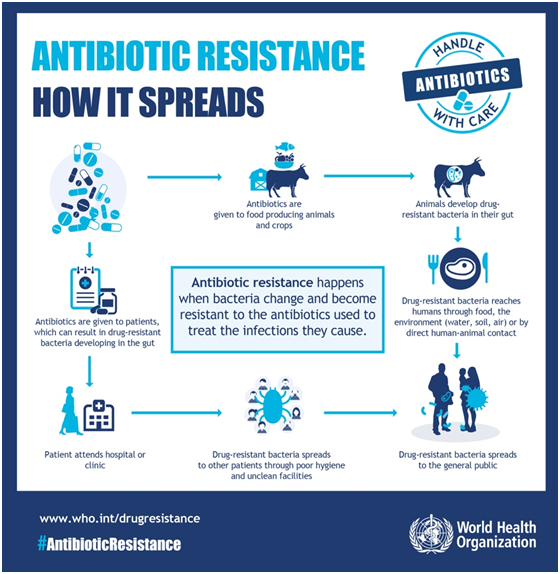
- Antimicrobial Resistance (AMR) occurs when bacteria, viruses, fungi and parasites change over time and no longer respond to medicines making infections harder to treat and increasing the risk of disease spread, severe illness and death.
- As a result of drug resistance, antibiotics and other antimicrobial medicines become ineffective and infections become increasingly difficult or impossible to treat.
- It is estimated that bacterial AMR was directly responsible for 1.27 million global deaths in 2019 and 4,95 million deaths were associated with drug resistant infections.
Causes of AMR:
- Selective pressure:
- In the presence of an antimicrobial, microbes are either killed or, if they carry resistance genes, survive.
- These survivors will replicate, and their progeny will quickly become the dominant type throughout the microbial population.
- Mutation:
- Most microbes reproduce by dividing every few hours, allowing them to evolve rapidly and adapt quickly to new environmental conditions.
- During replication, mutations arise and some of these mutations may help an individual microbe survive exposure to an antimicrobial.
- Inappropriate use:
- Unnecessary and injudicious use of antibiotic fixed dose combinations could lead to emergence of bacterial strains resistant to multiple antibiotics.
- Hospital use:
- Critically ill patients are more susceptible to infections and, thus, often require the aid of antimicrobials.
- However, extensive use of antimicrobials and close contact among sick patients creates a fertile environment for the spread of antimicrobial-resistant germs.
- Agricultural use:
- Scientists also believe that the practice of adding antibiotics to agricultural feed promotes drug resistance.
Intervention Strategies:
- The principles of infection prevention and control remain a foundation for preventing infections broadly and a cornerstone in combating the spread of AMR.
- Preventing infections through vaccinations is paramount for reducing the need for antibiotics.
- Reducing exposure to antibiotics unrelated to treating human disease is an important potential way to reduce risk.
- Increased use of antibiotics in farming has been identified as a potential contributor to AMR in humans.
- Minimising the use of antibiotics when they are not necessary to improve human health—such as treating viral infections—should be prioritised.
- To this end, building infrastructure that allows clinicians to diagnose infection accurately and rapidly is crucial so that antimicrobial use can be narrowed or stopped when appropriate.
- Maintaining investment in the development pipeline for new antibiotics—and access to second-line antibiotics in locations without widespread access—is essential.
Measures Taken by Govt. of India to Tackle AMR:
- Government is aware about the challenges posed by AMR in India and has taken following measures to address the issue:
- AMR surveillance network has been strengthened by establishing labs in State Medical College. 36 sites in 26 States/UTs have been included in this network so far.
- National action plan on containment of Antimicrobial Resistance (NAP-AMR) focusing on One Health approach was launched in 2017 with the aim of involving various stakeholder ministries/departments.
- AMR Surveillance Network: ICMR has established AMR surveillance and research network (AMRSN) comprising 30 tertiary care hospitals, both private and government to generate evidence and capture trends and patterns of drug resistant infections in the country.
- AMR Research & International Collaboration: ICMR has taken initiatives to develop new drugs /medicines through international collaborations in order to strengthen medical research in AMR.
- Red Line Campaign: The Union health ministry’s “Red Line Campaign” urges people not to use medicines marked with a red vertical line, including antibiotics, without a doctor’s prescription.
- This campaign is aimed at discouraging unnecessary prescription and over-the-counter sale of antibiotics causing drug resistance for several critical diseases including TB, malaria, urinary tract infection and even HIV.
News Summary:
- The Union Health Ministry has urged all doctors in medical colleges and medical associations to make it a mandatory practice to mention indication, reason for justification while prescribing antibiotics.
- Director General of Health Services has also appealed to all pharmacists to strictly implement schedule H and H1 of the Drugs and Cosmetics Rules and stop over-the-counter sale of antibiotics and sell them only on the prescription of a qualified doctor.
- under Drugs and Cosmetics Rules 1945, antibiotics are included in the list of drugs specified under Schedule H which are required to be sold by retail on the prescription of a Registered Medical Practitioner (RMP) only.
- Some high-end antibiotics are included in list of H1 drugs.









