Why in news?
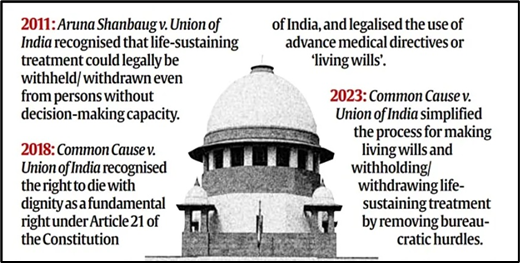
The Ministry of Health and Family Welfare has released draft guidelines to implement the Supreme Court's 2018 and 2023 orders on the right to die with dignity. These guidelines provide a framework for state governments and hospitals to withdraw life support for terminally ill patients.
Though India lacks specific legislation on life-sustaining treatment withdrawal, the guidelines affirm its legality within this regulated structure.
What’s in today’s article?
- Understanding Withholding or Withdrawing Life-Sustaining Treatment
- Euthanasia or the so called ‘mercy killing’ of a patient
- Living Will
- Medical Procedure for Withholding or Withdrawing Life-Sustaining Treatment
Understanding Withholding or Withdrawing Life-Sustaining Treatment
- About
- Withholding or withdrawing life-sustaining treatment involves ending medical interventions, such as ventilators and feeding tubes, when they no longer improve the patient’s condition or merely extend suffering.
- These treatments temporarily replace essential bodily functions but are discontinued to allow natural progression of the illness, providing comfort care and symptomatic relief instead.
- Right to Refuse Medical Treatment
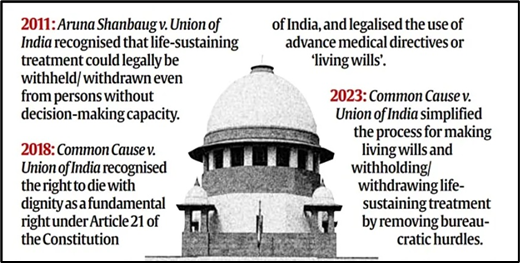
- The right to refuse medical treatment has long been upheld in common law and is recognized as a fundamental right under Article 21 (Right to life and personal liberty) of the Indian Constitution following the 2018 Supreme Court decision in Common Cause vs Union of India.
- This right allows patients to refuse life-sustaining treatments, even if refusal may lead to death.
- Process for Withholding or Withdrawing Life Support
- Through Patient Consent: If a patient has decision-making capacity, they can refuse treatment.
- Through Advance Directives or ‘Living Wills’: A patient may outline their wishes in a ‘living will’ to guide future medical care if they lose the ability to decide.
- For Patients Without Capacity or Living Will: In cases where a patient cannot make decisions and lacks a living will, the treating physician can recommend withholding or withdrawing treatment if there is no reasonable chance of recovery, and further intervention would only prolong dying.
Euthanasia or the so called ‘mercy killing’ of a patient
- Understanding Euthanasia and Misconceptions Around “Passive Euthanasia” in India
- Euthanasia involves the intentional ending of a terminally ill patient’s life by a doctor to relieve suffering.
- In India, “passive euthanasia” often refers to withholding or withdrawing life-sustaining treatment, but this term has led to misconceptions and public apprehension regarding the right to die with dignity.
- A 2018 glossary by the Indian Council of Medical Research highlighted that this term is widely misunderstood and lacks social acceptability.
- Withholding or Withdrawal of Life Support and Do-Not-Attempt-Resuscitation (DNAR) Orders
- The withdrawal of life-sustaining treatments can include “do-not-attempt-resuscitation” (DNAR) orders, where a physician decides, in consultation with the patient or family, not to attempt resuscitation.
- Importantly, DNAR does not mean stopping other medical treatment; it only limits resuscitation efforts.
- Does Withholding or Withdrawing Treatment Mean Giving Up on the Patient?
- Choosing not to continue life-sustaining treatment is not about abandoning the patient but about recognizing when interventions are futile and only prolong suffering.
- In such cases, the focus shifts to palliative care, ensuring the patient’s comfort.
- In contrast, discharging patients against medical advice often results in inadequate care, increasing suffering for patients and their families.
Living Will
- To support the right to die with dignity, the Supreme Court established guidelines in 2018 for creating living wills, later simplified in 2023.
- A living will allows individuals aged 18 or older to outline their medical care preferences should they lose decision-making capacity.
- The document must name at least two trusted surrogate decision-makers.
- To be legally binding, it must be signed before an executor, two witnesses, and attested by a notary or gazetted officer.
Medical Procedure for Withholding or Withdrawing Life-Sustaining Treatment
- Guidelines by SC
- The Supreme Court's guidelines outlined a structured procedure for withholding or withdrawing life-sustaining treatment.
- It emphasized the rights and duties of both doctors and patients and ensuring independent expert assessment and consent from family or surrogate decision-makers.
- Primary Medical Board Assessment
- A Primary Medical Board, consisting of the treating doctor and two subject-matter experts with a minimum of five years’ experience, is constituted by the hospital.
- This board assesses the patient’s condition and determine the appropriateness of stopping life-sustaining treatment.
- Secondary Medical Board Review
- For additional oversight, a Secondary Medical Board is set up to review the Primary Board’s decision.
- It includes a registered medical practitioner appointed by the district Chief Medical Officer and two experienced subject-matter experts, all different from those on the Primary Board.
- Consent from Family or Surrogate Decision-Makers
- Consent from the patient’s nominated representatives in an advance directive or, where unavailable, surrogate decision-makers is required before withholding or withdrawing treatment.
- Judicial Notification
- The hospital must notify the local judicial magistrate about the decision to withhold or withdraw life-sustaining treatment.
- Shared Decision-Making and Ethical Responsibility of Doctors
- The procedure promotes “shared decision-making,” involving the medical team and the patient’s family or surrogates to jointly agree on treatment decisions.
- This protects doctors legally, respects patient autonomy, includes family wishes, and maintains ethical standards without placing sole responsibility on the physician.