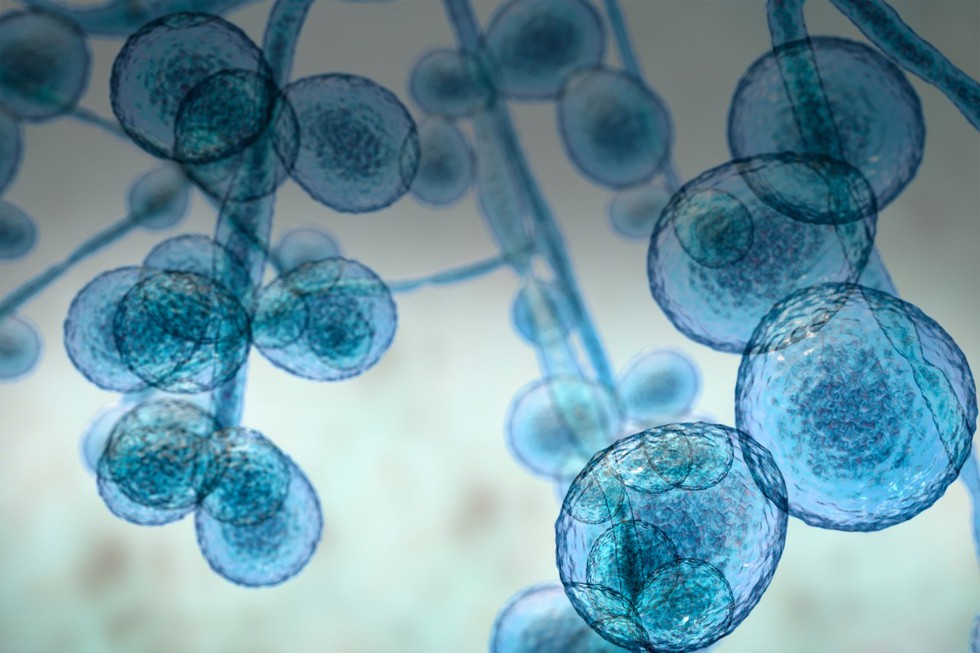
About Candida Auris (C. auris):
- It is a fungal pathogen that is often multi-drug-resistant.
- It is capable of causing invasive infectionsin the human body.
- It can cause a range of infections, from superficial (skin) infections to more severe, life-threatening infections, such as bloodstream infections.
- It can cause infection in different parts of the body, like the blood, wounds and ears.
- It was first identified in Japan in 2009.
- How is it contracted?
- Most casesof the fungus have been reported in healthcare settings, such as hospitals and nursing homes.
- It is generally thought to be spread through contact with contaminated surfaces or by person-to-person transmission.
- People who are already suffering from other medical conditions, recent hospital stays, and invasive devices are most at risk of contracting the fungus.
- How does the fungus act on the body?
- There are two ways C. auris can affect the body:
- The fungus can either live on a specific region, such as the skin, rectum, or mouth, in a process called “asymptomatic colonization,” where a patient has no symptoms but can spread it to other people.
- It can enter the bloodstream or wounds, where it can cause severe invasive infections.
- Symptoms:
- Its symptoms are often similar to those of other common diseases and hence diagnosis is difficult.
- The most common symptoms of C. auris include fever and chills that don’t go away after treatment with antibiotics.
- Mortality Rate: It is estimated to be between 30-60%.
- Treatment:
- Most C. auris infections are treatable with antifungal drugs called echinocandis.
- However, some C. auris infections are resistant to the main types of antifungal medications, making them more difficult to treat.
- In this situation, multiple antifungals at high doses may be required to treat the infection.